I made a flowchart of sorts for my treatment, because, well, it’s me.
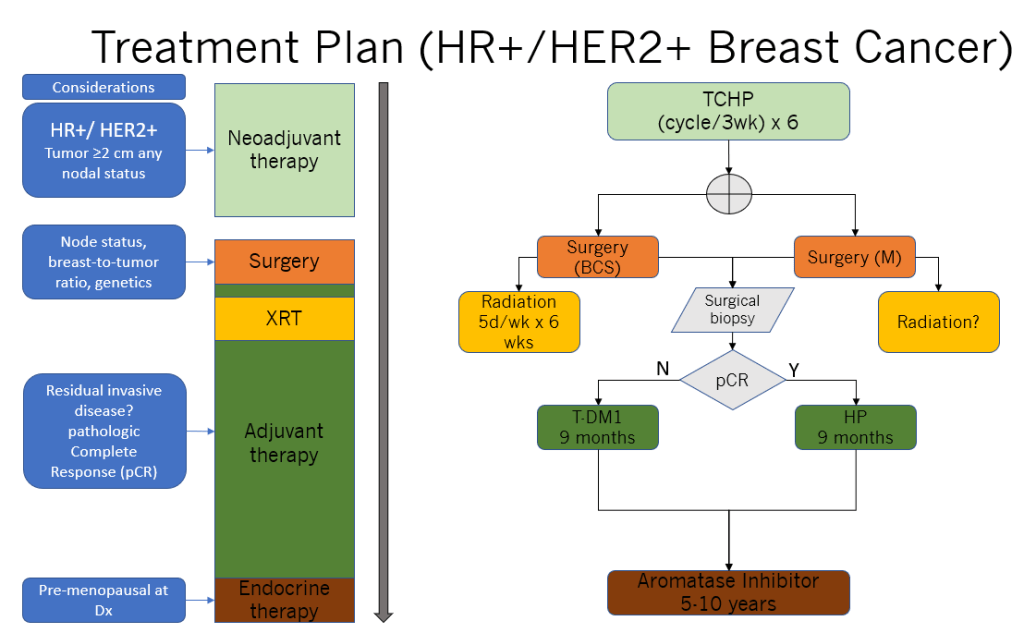
By August 26 officially (or even before that, unofficially), I knew what the treatment plan was going to be for my cancer. Nothing was going to be unprecedented, or out of the ordinary. I knew we would start with neoadjuvant therapy for 6 cycles at 3 weeks apart, and we would start as early as beginning of September. So I spent the last couple of weeks preparing: cutting my hair, purchasing some OTCs known to help with the side effects, doing some serious laundry, and informing family, friends, colleagues.
For the treatment to start, we had to get my port-a-cath (infusion port) installed on my chest by an Interventional Radiologist (IR). As apprehensive as I was about this, this minor surgery wasn’t complicated. I did get a great deal of nausea and vomiting and dizziness at recovery. Unsure why. The combination of sedation and pain medication has resulted in some complications for me in the past (previous surgery), but it wasn’t of grave concern. It just made for great discomfort to me. The port healed just fine and I was pleased it was available for me on my 1st infusion.

If it seems I went from zero to 60, diagnosis to treatment, assuredly, I didn’t. It was fast, but there were many steps I’d had to take over a period of 4 weeks, including:
- A diagnostic mammogram
- An ultrasound
- A Fine Needle Aspiration (FNA) Biopsy, 2x
- A core biopsy
- An echocardiogram and EKG
- MRI
- A CT scan
- An NM bone scan
- Another MRI
- Bloodwork
- Genetic testing
- And a consult with the surgical oncology team
Currently I am under the care of the medical oncology team headed by my oncologist, Dr H. Throughout this chemotherapy and immunotherapy, they are my partners in ensuring I have my labs, my infusion schedule, my concerns alleviated and my questions answered.
